Table of Contents
Medicaid is a vital program that helps millions of Americans get access to essential healthcare services, including transportation. But when it comes to non-emergency transportation (NEMT), many people are left wondering: How much does Medicaid pay for non-emergency transport? It’s not as simple as you may assume to answer that. In this article, we will uncover the hidden facts about Medicaid’s coverage for non-emergency transport, giving you a clearer understanding of what to expect.
What is Non-Emergency Medical Transportation (NEMT)?
Understanding Non-Emergency Medical Transportation
Non-Emergency Medical Transportation (NEMT) is a service covered by Medicaid that helps people who don’t have access to reliable transportation get to and from medical appointments. This includes rides to doctors, clinics, hospitals, and therapy sessions. Unlike emergency transport (like an ambulance), NEMT is used for routine, non-life-threatening medical visits.
Why NEMT is Important
NEMT is a crucial service for low-income individuals, elderly patients, and people with disabilities who may not have the means to drive themselves or access public transportation. Without NEMT, many Medicaid recipients could miss essential appointments, leading to worsening health conditions and higher medical costs in the long run.
How Medicaid Determines NEMT Coverage
How Much Does Medicaid Pay for Non-Emergency Transport?
When asked, How much does Medicaid pay for non-emergency transport? A few crucial elements determine the response. Medicaid operates differently in each state, and coverage policies can vary widely. However, some general guidelines help determine how much Medicaid pays for these services.
State-Specific Medicaid Programs
Medicaid is a federal program, but each state runs its version, which means the rules about what services are covered, including NEMT, can differ. Most states cover the total cost of non-emergency transportation for Medicaid recipients, while others might have a cap on the number of trips or specific mileage limits.
What Does Medicaid Pay for NEMT?
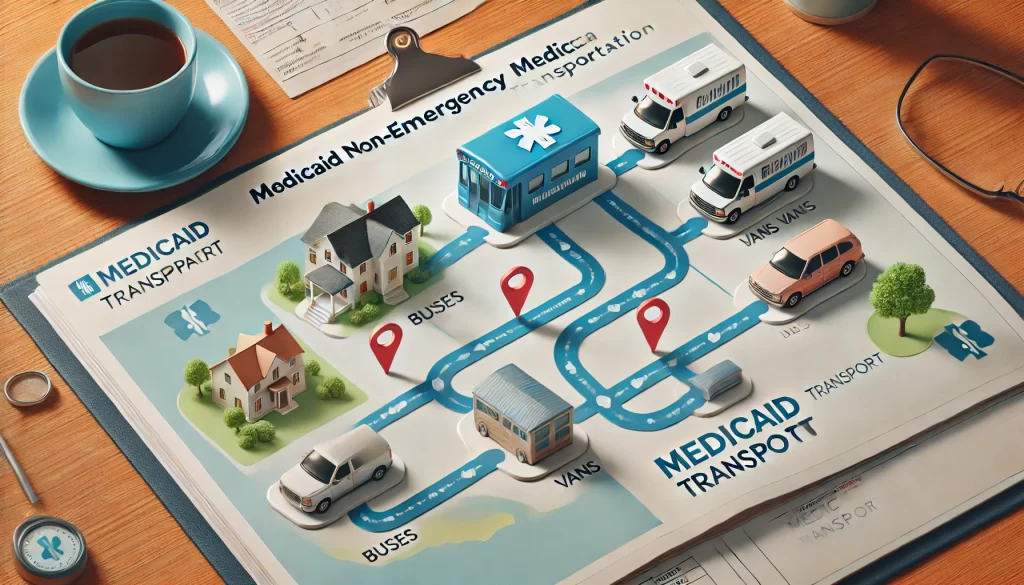
Medicaid generally covers the total cost of approved NEMT services. This can include:
- Rides provided by professional transportation companies
- Reimbursement for mileage if a friend or family member drives you
- The cost of public transportation, like buses or trains
However, some states may require a small co-pay for each ride, typically ranging from $1 to $5. It’s essential to check with your state’s Medicaid office to know the exact rules for NEMT coverage in your area.
Factors That Impact Medicaid NEMT Payments
What Affects Medicaid Coverage for NEMT?
Several factors determine how much Medicaid pays for non-emergency transport. Let’s break down the most important ones:
Type of Transportation
Medicaid covers different types of non-emergency transport based on the patient’s needs. Some patients require a simple car ride, while others may need wheelchair-accessible vans or even stretcher transport. The type of vehicle required directly impacts the cost Medicaid will cover.
Distance of Travel
The distance you travel for medical appointments can also affect how much Medicaid will pay. Longer trips may require more reimbursement or coverage. For instance, if you live in a rural area far from medical facilities, Medicaid may cover a greater portion of the cost due to the increased distance.
Number of Appointments
Some states limit the number of NEMT trips covered per month. For example, Medicaid may only cover four round trips to medical appointments each month. If you exceed that limit, you might have to pay for extra rides out of pocket. Check with your state’s Medicaid program to understand any limitations.
How to Apply for Medicaid NEMT Services
Getting Medicaid Non-Emergency Transportation
Knowing how much Medicaid pays for non-emergency transport is only part of the puzzle. To actually receive NEMT services, you need to follow a few steps:
Step 1: Contact Your Medicaid Provider
Your first step is to contact your state’s Medicaid office or your managed care provider. They will let you know what services are available and how to schedule a ride.
H3: Step 2: Get Pre-Authorization
Many states require pre-authorization before you can use NEMT services. This means your doctor will need to confirm that you need transportation to your medical appointments.
Step 3: Schedule Your Ride
Once you’re approved, you can schedule a ride. Depending on your state’s Medicaid program, you may have the option to choose from a list of transportation providers or use an app to book your ride. In some cases, Medicaid will reimburse you for transportation expenses if you or someone you know drives you to your appointment.
Also Read: How Much Does Medicaid Pay for a Caregiver? Shocking Facts Revealed!
The Hidden Facts of Medicaid NEMT
The Truth Behind Medicaid NEMT Payments
While Medicaid covers non-emergency transportation, it’s essential to know that there are limits and conditions to this coverage. How much does Medicaid pay for non-emergency transport? It depends mainly on your state’s policies, the distance to your appointments, and the type of transport you need. Medicaid aims to ensure that all recipients can access necessary medical care, but the actual payments and coverage vary widely.
Hidden Costs and Limitations
While Medicaid covers most transportation expenses, there are hidden factors you should be aware of. For example:
- Some states limit the number of rides you can take.
- Medicaid may not cover trips if the appointment is considered non-essential.
- You may have to pay small co-pays for each ride.
Understanding these limitations can help you plan your medical appointments and transportation needs more effectively.
How much does Medicaid pay for non-emergency transport varies by state, the distance you travel, and the type of transportation you require. While Medicaid covers many transportation costs, there are important factors and limitations to consider. To make sure you’re getting the most out of Medicaid’s NEMT services, stay informed about your state’s specific rules, and don’t hesitate to reach out to your Medicaid provider for guidance.
By understanding these hidden facts, you can better navigate the Medicaid system and ensure that you receive the transportation services you need without surprises.